Overview
Background
Although an essential component of all routine physical examinations, the physical examination of the abdomen is the key step in the evaluation of abdominal complaints such as pain, distension, enlarged organs, or masses.
The examination is conducted in a predetermined sequence starting from observation and then sequentially performing auscultation, palpation, and percussion (see images below) followed by ancillary maneuvers. However, a vital step in assuring a successful outcome is to properly prepare the challenging patient before anything else is done. For children, the parents should be present; if additional individuals are in the examining room, then the child must feel comfortable with their gender and their inclusion. The astute clinician must have specific goals in mind based on the history obtained. Like a musician or a dancer performing the same routine, the experienced caregiver can make subtle adjustments to yield the optimal result depending on the circumstances.
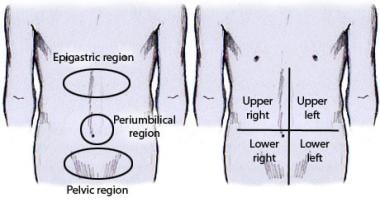
The most common reason for performing a focused examination is to identify the etiology of abdominal pain, which can be subdivided into visceral, somatoparietal, or referred. By definition, visceral pain cannot be specifically localized; however, accurate deductions can be drawn from a complete examination. Lower esophageal, gastric, and duodenal discomforts are best appreciated in the epigastric area. Signs of distal small bowel and/or colonic distension are usually expressed in the periumbilical region. Lower quadrant findings are typically secondary to pathology involving the ileocecum and appendix in the right and the rectosigmoid on the left. Somatoparietal findings correspond more exactly to the precise underlying abdominal contents.
Although the abdominal examination has been a well described and fundamental component of a systematic diagnostic evaluation since antiquity, its role in modern medicine is being minimized. Unfortunately, most of the recent editions of standard textbooks of pediatrics, and of pediatric and adult gastroenterology do not emphasize this activity. The reader must instead consult textbooks devoted primarily to physical examination for additional descriptions of this process. [1] Cope’s classic treatise on the acute abdomen remains an excellent resource for a comprehensive explanation of performing the examination in adults and integrating it into patient care. [2]
In the United States, Western Europe, and most of the developed world, the role of the examination has been supplanted by high-resolution imaging techniques that are widely available. A cross-sectional study of 26 million pediatric emergency department visits revealed that, overall, the rate of advanced imaging increased from 6.4% of encounters in 2009 to 8.7% in 2018; specifically, the rate of computed tomography decreased from 3.9% to 2.9%, the rate of ultrasonography increased from 2.5% to 5.8%, and the rate of magnetic resonance imaging increased from 0.3% to 0.6%. [3]
The practice of greater reliance on radiographic findings has had many consequences. Patient outcomes become more dependent upon the technical quality of the study, which is dependent on the machine, the technician, and patient artifact, and the experience of the physician available to interpret the investigation during an emergency situation. This trend has also led to additional unnecessary radiation exposure as well as additional painful procedures (ranging from phlebotomy to invasive interventions) to characterize unanticipated abnormal radiographic findings and has also significantly contributed to the spiraling cost of health care in many countries. [4]
A large cross-sectional study has proposed a scoring system that would utilize a few standard screening laboratories in conjunction with a detailed physical examination to decrease the number of pediatric CT scans after blunt abdominal trauma. [5] One publication highlighted that inadequacies in performing and interpreting the physical examination have contributed to medical error. [6] With the decreased utilization of routine abdominal examination in clinical medicine in the twenty-first century, there has been a decreased emphasis on teaching these skills. Paradoxically, the use of point-of-care ultrasounds has been introduced into medical schools to assist the teaching of physical examinations, particularly examinations of the cardiovascular system and the abdomen. [7]
Performing an abdominal examination in children is more challenging than in adults. A review article examining the published literature on diagnosing pediatric appendicitis failed to find a single study that documented that physical examination provided an acceptable level of sensitivity and specificity to arrive at a correct diagnosis. [8] The cardinal finding of right-lower quadrant pain predicts appendicitis more accurately in adults than in children. However, the authors still concluded that "clinical examination plays a key part in determining which children with abdominal pain should undergo immediate surgical consultation for appendectomy and which children should undergo further diagnostic evaluation, including diagnostic imaging." [8]
Indications
The abdominal examination is part of all comprehensive examinations of all patients of all ages. These may be routine, scheduled examinations, or examinations to address nonspecific symptoms such as fever, weight loss, lethargy, loss of appetite, and nausea. It is an essential component of the evaluation of the patient with abdominal trauma (see images below), or generalized trauma which may include abdominal organs. It is the primary focus of the evaluation of a patient whose chief symptom is related to any type of abdominal signs or symptoms including, but not limited to, the terms listed above and to any suspected pathology in the gastrointestinal tract. If life-threatening intestinal pathology exists, most commonly obstruction, perforation, ischemia, or volvulus, a rapid and diagnostic abdominal examination will be the single most important factor to avoid mortality and to minimize morbidity.
 Abdominal wall findings in a passenger who was restrained with only a lap belt during a motor vehicle accident.
Abdominal wall findings in a passenger who was restrained with only a lap belt during a motor vehicle accident.
Contraindications
No contraindications exist to performing an abdominal examination. When significant pain exists, such as in the patient who is experiencing peritoneal irritation, ischemia of either the intestine or an abdominal organ (testes, ovary, spleen), or stretching of the capsule of the liver or kidney, the examiner should use a markedly gentler approach, which will be sufficient to elucidate the pathology. When splenomegaly exists, the examiner must exercise caution to avoid iatrogenic splenic injury.
Relevant Anatomy
The abdominal cavity is the largest hollow space in the body. It is bound cranially by the xiphoid process of the sternum and the costal cartilages of ribs 7-10; caudally, by the anterior ilium and the pubic bone of the pelvis; anteriorly, by the abdominal wall musculature; and posteriorly, by the L1-L5 vertebrae.
The anatomic planes of the abdominal wall are made up of multiple muscular and fascial layers that interdigitate and unite to form a sturdy, protective musculofascial layer that protects the visceral organs and provides strength and stability to the body's trunk.
The abdominal wall is composed of 5 paired muscles: 2 vertical muscles (the rectus abdominis and the pyramidalis) and 3 layered, flat muscles (the external abdominal oblique, the internal abdominal oblique, and the transversus abdominis muscles). These muscles and their fascial attachments interdigitate and unite to form a sturdy, protective musculofascial layer that gives strength and support to the anterolateral abdominal wall.
For more information about the relevant anatomy, see Regions and Planes of the Abdomen.
Preparation
Anesthesia
No pharmacologic agents are ever required to perform an abdominal examination. Sedative medications can mask worsening abdominal symptoms. They may delay an urgent surgical intervention and are therefore contraindicated in this setting. However, proper preparation of the young child or anxious patient is a crucial first step in performing a successful examination.
The examiner must have a calm approach and create an empathetic and confident atmosphere to gain the trust of the challenging patient prior to initiating physical contact. Verbal distraction is a valuable technique to enable a full examination, especially in the uncooperative child. [8] Children should be asked age-appropriate, engaging questions that they can focus on such as “Do you watch TV? What is your favorite TV show?”, “What is the name of your teacher? What games do you like to play in school?”, or “What was the funniest thing that happened in school today?”
Positioning
Abdominal examination is ideally performed with the patient in the supine position. The examiner should first observe the anxious patient and have him or her calm down enough to assess any evidence of tenderness prior to initiation of auscultation and palpation. For younger children who remain distraught, the examination can be performed with the patient in the mother’s lap. [8] In other situations, the examiner should be on the patient’s right side so that the liver is easily accessible without reaching over.
Complication prevention
No complications result from this procedure and no special measures need to be taken.
Examiner preparation
The key to a successful outcome for an abdominal examination is the thought process of the examiner prior to starting the procedure. The abdominal examination is always a step-wise procedure, and the experienced practitioner should follow the same sequence for all patients, using age-specific modifications to achieve the desired goals. A long list of differential entities can be the cause of abdominal pain; these are well described in standard text books and recent reviews. [9, 10, 11]
Consequently, a complete history should be obtained, and a set of probable diagnostic possibilities should be entertained prior to starting the examination. One useful categorization is described in Table 1 that has been adapted by the authors from several sources. [9, 10, 11] The history should include characterization of the time frame, subjective description, severity, pattern, and location of the pain and other complaints.
Additional essential history would include presence of weight gain or loss, nausea and/or vomiting, change in bowel movements, rectal bleeding, jaundice, abdominal distension, and pruritus. Symptoms suggestive of an urgent, surgical, problem represent a different set of possibilities than those that are consistent with a chronic condition. Similarly, the patient who presents with marked morbidity should suggest different conditions from the one with subjective rather than objective complaints.
Table 1. Commonly Encountered Etiologies of Abdominal Pain in Children Arranged by Age and Characteristics (Open Table in a new window)
|
Infancy (< 2 y) |
Preschool Age (2-5 y) |
School Age (>5 y) |
Adolescent |
Gastrointestinal |
|
|
|
|
Surgical abdominopelvic emergencies |
|
|
|
|
Extra-abdominal |
|
|
|
|
In each box the most commonly encountered etiologies are marked with an asterisk (*). All entities that have a characteristic location have these identified: E= epigastric; RU = right upper quadrant; RL = right lower quadrant; RL = right lower quadrant; LL = left lower quadrant; P = periumbilical; D = diffuse; S = subxiphoid; RLLQ = either right or left lower quadrant; RLUQ = either right or left upper quadrant; IBD = inflammatory bowel disease; IBS = Irritable bowel syndrome; UTI = urinary tract infection; AGE = acute gastroenteritis; acid peptic disease = (reflux esophagitis, gastritis, duodenitis, peptic ulcer); colonic distension (secondary to carbohydrate ie lactose, sucrose, sorbitol malabsorption)
Based on the assessment, the examiner should begin with diagnostic possibilities that can be supported or decreased in likelihood by the examination (see Table 2). In all cases, and especially if the history fails to provide specific clues, the examiner should be aware of the common diseases that manifest with abdominal symptoms and should then try to determine if any physical findings consistent with these entities are present. A child with chronic constipation should not be subjected to appendectomy because of severe pain related to colonic distension when they arrive in the emergency room.
Table 2. Correlation of Physical Findings With Diagnostic Possibilities (Open Table in a new window)
Physical Finding |
Disease Process to Consider |
Epigastric tenderness |
Acid peptic disease (GER, gastritis, PUD) |
Discomfort with minimal movement |
Peritonitis |
Distension with fullness left lower quadrant |
constipation |
Diffuse tenderness with increased tympany |
IBS vs small bowel obstruction |
Tenderness at McBurney's point |
Appendicitis |
Tenderness medial to McBurney's point |
Meckels diverticulum |
Increased tenderness with inspiration in RUQ (Murphy sign) |
Gallbladder pathology |
Pain with lifting extended right leg against resistance (Psoas sign) |
Retrocecal appendicitis or other retroperitoneal irritation (abscess of Crohn disease, pancreatitis, pyelonephritis) |
Bulging flanks |
Ascites or obesity |
Shifting dullness |
Ascites |
Pain with deep knee squats |
Retrocecal appendicitis |
"Hepatosplenomegaly" with cephalad borders at lower ribs |
Hyperinflation as seen in obstructive pulmonary disease |
Hepatomegaly or hepatosplenomegaly with jaundice and/or caput medusae |
Cirrhosis with portal hypertension |
Hepatomegaly or hepatosplenomegaly without jaundice and normal consistency of enlarged organs |
Congestion secondary to heart failure |
Hepatomegaly or hepatosplenomegaly without jaundice and firm consistency of enlarged organs |
Storage or Infiltrative disease process including leukemia and other neoplasia |
Firm hepatomegaly without splenomegaly or jaundice, especially with increased blood pressure |
Congenital hepatic fibrosis |
Jaundice with liver tenderness, and/or enlargement |
Hepatitis |
Jaundice with normal liver findings |
Gilbert syndrome, hemolytic process, metabolic disease, early hepatitis |
Pain relieved by sitting up |
Pancreatitis, retroperitoneal pathology |
Periumbilical bruising and edema (Cullen's sign) |
Hemorrhagic pancreatitis |
Bruising of flanks (Grey Turner sign) |
Hemorrhagic pancreatic, renal hemorrhage |
Isolated splenomegaly |
Splenic trauma, extra-hepatic portal hypertension, splenic sequestration, hemolytic diseases, certain storage diseases |
Technique
Overview
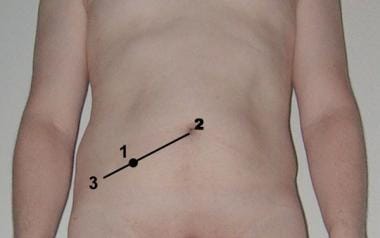
The patient should be exposed from the nipple line to the lower abdomen and lying supine. Flexing the knees slightly to relax the abdominal musculature is sometimes helpful. The abdomen can be divided into 4 quadrants, with vertical and horizontal lines intersecting at the umbilicus. The quadrants are then named in clockwise direction: right upper, left upper, left lower and right lower quadrants. Other anatomical landmarks such as epigastric, periumbilical, suprapubic, and McBurney point (1/3 of the distance from the right anterior superior iliac spine to the umbilicus) should be referenced to provide additional details. See images below.
All physical findings should be related to the area in which they are located. After the patient has been placed in the proper position, the examiner begins by observing the abdomen for any asymmetry and to detect any distension. The presence or absence of scars can provide clues and in certain cases may clarify the history if the patient is unclear or unable to provide accurate information. Bulging flanks suggest the presence of ascites or obesity. Signs of liver disease (tortuous abdominal vessels or jaundice) or pancreatic hemorrhage (Grey Turner and Cullen signs) may be evident. [12] See images below.
 Grey Turner sign. This 40-year-old woman complained of worsening epigastric pain of five days' duration. On examination, she had hypotension, a board-like abdomen, and extensive ecchymoses over her right loin.
Grey Turner sign. This 40-year-old woman complained of worsening epigastric pain of five days' duration. On examination, she had hypotension, a board-like abdomen, and extensive ecchymoses over her right loin.
All physical signs must be interpreted with the patient’s age in mind because the differential may change drastically. For example, the presence of a scaphoid abdomen in a neonate with respiratory distress may indicate diaphragmatic hernia, but not in an older child. [13] Also in the newborn, the appearance or persistence of the umbilical stump may generate clues to a source of fever, to an underlying immunological disorder, or to liver or pancreatic disease. [13] A patient that is afraid of excessive movements may be experiencing peritoneal irritation. A young child or infant who experiences discomfort lying down may be experiencing gastroesophageal reflux. In an older child, a preference for sitting up can indicate retroperitoneal irritation, as in pancreatitis.
The next step should be auscultation (see image below) for the presence and quality of bowel sounds prior to any other form of manipulation. As these sounds are audible throughout the abdomen and peristaltic activity is never restricted to one portion of the abdomen, the practice of auscultating in all 4 quadrants provides little useful information. In the younger child, bowel sounds can appear to be referred and attempting to draw conclusions based on the apparent area of auscultation can be misleading. If bowel sounds are not immediately audible, a period of 30-60 seconds should be dedicated to listening as the establishment of absent bowel sounds has immediate implications and should be unequivocal. High-pitched, frequent bowel sounds are associated with small bowel obstruction. Abdominal bruits are associated with vascular, most commonly large arterial, pathology.
Initially, gentle palpation should determine the context for further examination by determining if peritoneal signs and exquisite tenderness exist and whether the pertinent findings are general or localized. The examiner should focus on the child’s face to detect nonverbal indicators of tenderness. [8] Palpation should always begin with light, soft, circular movements and should start in the area away from the suspected pathology. In this manner, the examiner can establish that portions of the abdomen are free from tenderness and apparent pathology.
As each region is examined, the contents and their potential for pathology should be sequentially palpated. For the solid organs of the abdomen, the liver, the spleen, and any masses, the perimeters of the structure should be defined and a quantitative estimate of the dimensions should be determined and recorded. Hepatomegaly without jaundice should prompt the consideration of storage rather than inflammatory liver disease. The surface should be repeatedly felt to establish whether the structure is homogenous and whether the surface is smooth, irregular, or nodular in addition to defining if it is tender. The qualitative and quantitative findings should be put into a well-defined, reproducible, anatomic context.
The span of the liver, for example, should be measured in the right midclavicular line. Presence of splenomegaly begins with gentle palpation from the umbilicus in an upward diagonal direction into the left upper quadrant. Support of the flank on the left may support and aid in projection of the spleen toward the examiners fingers. Enlarged or cystic kidneys may also be palpated with this maneuver. [1] It should be noted if the spleen, the liver, or both cross the midline.
Percussion of intercostals spaces is required to determine the cephalad border of the liver and of the spleen and thus to unequivocally establish the presence of organomegaly. Percussion is performed by tapping on the examiner’s hand with the second digit of the other hand. It may be an invaluable maneuver to determine size. The caregiver should be able to distinguish between hyperinflation of the lungs (as seen in asthma or cystic fibrosis or any obstructive pulmonary disease) from true hepatosplenomegaly. If the latter is present, the examiner should attempt to determine if the enlarged organs are firm and/or heterogeneous from an infiltrative process or have a normal consistency from congestion (see Table 2 in Preparation).
If determining the size of the liver is difficult, the scratch test may provide additional information. The diaphragm of the stethoscope is held over the liver, and the examiner listens for change in the quality of sound as the opposite hand gently scratches the abdomen moving in a semicircle around the stethoscope. [1]
Tenderness medial to McBurney’s point suggesting a Meckel diverticulum should be distinguished from typical appendicitis tenderness. The presence of dilated loops of bowel by palpation or percussion is an important finding that should be sought along with the degree of tenderness associated with the distended bowel. If tenderness is appreciated in an area of the abdomen that is unusual or does not match the history, then gentle pinching of the abdominal muscles should be performed to determine whether the pathology is actually musculoskeletal rather than abdominal. Regardless of the initial findings, all 4 quadrants, with particular attention to the liver, spleen, and any areas of fullness or symptoms, should be sequentially examined and the findings recorded.
Dullness along the flanks while in the supine position may indicate the presence of ascites. Various maneuvers can confirm this finding. [14] The examiner should percuss from the midline laterally and if ascites is present, a change from the tympany of bowel gas to the dullness of fluids should exist. The patient should then be positioned in a lateral position and the same sequence should be performed. If free-flowing ascitic fluid exists, the gravity will reposition it to the dependent side and a “shifting dullness” will be present.
The older, cooperative child or the parent can put the sides of their hands by the umbilicus, perpendicular to the abdomen, and apply gentle pressure. The examiner then gently pushes on one flank and determines if the “fluid wave” can be palpated on the opposite side. The “puddle sign” may also be used in children by first percussing the umbilicus while supine. As the child is moved to a prone position the ascitic fluid pools anteriorly, and the acoustic quality of percussion changes. The child may be placed in this position either by holding a very small child prone or by having them support themselves on their hands and knees.
Frequently, ancillary maneuvers are required to arrive at a diagnosis. Asking the patient to breathe in while gently pushing on the abdomen and then observing the response to rapid removal of the hands is an indication of rebound tenderness or peritoneal irritation. For a more anxious child, gently moving the feet or the bed may yield the same response. [8] If this finding is limited to the right upper quadrant (Murphy’s sign), it supports the presence of biliary disease. Eliciting pain by raising the right leg against pressure supplied by the examiner’s hand while in the supine position suggests psoas irritation. Besides providing the hallmark of appendicitis, it may suggest other, less common, retroperitoneal conditions (see Table 2 in Preparation).
Demonstrating pain with hopping, especially in a younger child, suggests peritoneal irritation. This may be an early sign of appendicitis, a diagnosis commonly missed in the young child. The most important of the ancillary maneuvers performed in conjunction with an abdominal examination is a rectal examination.
Inspection of the perineum for rashes, gluteal wasting, gluteal asymmetry, perianal disease, fistulas, areas of fluctuance, and fissures often yields important findings. If a digital examination is performed, anorectal stenoses, the presence and the consistency of stool, the presence and an estimation of the size of any polyps or other masses, stool guaiac, and tenderness should be recorded. If the patient has a history of constipation, a Valsalva should be performed to help address the contribution of dyschezia to the symptoms. If appendicitis is suspected, a bimanual examination should be performed during the rectal to assist in the diagnosis of retrocecal inflammation, which may otherwise be unappreciated. It has been suggested that abdominal pain with deep knee squats can also help to diagnose retrocecal appendicitis. [8]
If an abdominal examination is considered part of the art of medicine, it is becoming a lost art. Subtle pathology, such as hypertrophic pyloric stenosis, will usually require several minutes dedicated to gentle palpation with the baby in the mother’s lap in order to relax the abdominal muscles and appreciate the olive-shaped mass. Starting 10-15 years ago, experienced pediatric surgeons began to lament a substantially higher reliance on ultrasound rather than abdominal examination to diagnose this entity and reported the additional costs involved in this transition. [15] More recently, this trend has continued with reports on how efficiently pediatric surgeons can perform the diagnostic ultrasound themselves. [16]
At the conclusion of the examination, the practitioner should have a strong opinion on the urgency of the situation and have a clear idea on the progression of further diagnostic investigations that are required to reach a definitive diagnosis. If either of these parameters cannot be fulfilled, a more experienced clinician should be immediately called upon to avoid unnecessary delays. As the signs and symptoms of a surgical condition can be evolving over time, admission for serial examinations is an acceptable course of action. However, an objective, quantitative, or semi-quantitative (eg, moderate severe pain, 6/10 tenderness) assessment should be documented to allow for other care givers to participate in optimal sequential assessments. This is especially crucial if the patient is being moved between locations, ie, from the emergency room to the ward, from the ward to the intensive care unit, or from the recovery room to the inpatient observation ward.
After any abdominal surgery, serial physical examinations are mandatory to recognize the onset of complications. Although postoperative pain and analgesia are expected, subtle indicators of increasing pain or generalized peritoneal irritation should be sought in regular intervals. If discovered, early radiographic and laboratory investigations should be obtained to minimize morbidity and mortality.
Post-Procedure
Follow-up, including long-term monitoring
Unless a completely unremarkable examination is identified and an alternative source of the patient’s complaints is established, or a surgically correctible condition is operated on, patients will require medical follow-up after a diagnostic abdominal examination. The time frame and the nature of the follow up will be dictated by the findings. A patient with an exacerbation of their inflammatory bowel disease or with abdominal trauma usually requires hospitalization for close monitoring that will include serial examinations starting in a few hours. Patients with mild acid peptic disease, constipation, or irritable bowel syndrome (the most commonly diagnosed conditions as well as the most significant contributors to functional abdominal pain in children) will need to be seen after several weeks to determine the efficacy of the dietary, pharmacologic, and life style changes that were originally proposed.
Patient education
The provider should explain thoroughly the importance of all of the therapeutic interventions that are offered to maximize the likelihood of full compliance and the resolution of the symptoms. For chronic problems, the long-term commitment to adhere to the therapeutic program, including ethanol abstinence for hepatitis and pancreatitis, avoidance of NSAIDs for acid peptic disease, compliance with pharmacologic regimens for inflammatory bowel disease, and a high-fiber diet for constipation, are the final steps in a successful therapeutic abdominal examination.
Tests and Medications
Often, the patient with abdominal pathology requires diagnostic investigations to confirm the physical findings from an examination as well as to quantitatively measure the pathology. For issues that require characterization of an anatomic entity, such as hepatomegaly, abdominal mass, biliary colic, or ovarian cyst(s), an abdominal, and perhaps pelvic, sonogram is an inexpensive, safe initial investigation.
If further definition is required or if the operator is inexperienced, then either a CT scan or MRI can be performed. This will depend on the availability of the equipment, the radiologist, and the personnel to provide adequate and safe sedation, if required. Laboratory investigations should be used judiciously and includes a CBC count (to evaluate for evidence of inflammation and/or bleeding), a comprehensive metabolic profile (to evaluate for hepatic, renal dysfunction), calculation of an anion gap (to evaluate for ischemia, diabetic ketoacidosis, ingestions, inborn errors of metabolism or sepsis) (see the Anion Gap calculator), an amylase (to evaluate for pancreatitis), and an ESR (marker for inflammation including infection, neoplasia, vasculitis, autoimmune phenomenon). A urinanalysis is required to diagnose urinary tract infection, calculi, and trauma.
Although no medications are required during or related to the performance of the abdominal examination, specific diagnoses based on the physical examination may require pharmacologic agents in order to resolve. These are discussed in the individual disease sections.
Questions & Answers
Overview
Why is a focused abdominal exam performed?
Why is the role of abdominal exam in the US and Western Europe being minimized?
What consequences have resulted from a diminished role of the abdominal exam?
How accurate is abdominal exam in diagnosing pediatric appendicitis?
What are the indications for abdominal exam?
What are the contraindications for abdominal exam?
What is the anatomy of the abdominal cavity relevant to an abdominal exam?
What is the role of anesthesia in an abdominal exam?
How is the patient positioned for an abdominal exam?
What are the possible complications of an abdominal exam?
What preparation is needed before an abdominal exam is performed?
What is the correlation between the physical findings and diagnosis following an abdominal exam?
What are the initial steps in an abdominal exam?
How is auscultation performed in an abdominal exam?
How is palpation performed in an abdominal exam?
How is the liver assessed in an abdominal exam?
How is a Meckel diverticulum differentiated from appendicitis during an abdominal exam?
How is the presence of ascites detected during an abdominal exam?
Which ancillary maneuvers may be required in an abdominal exam?
How is hypertrophic pyloric stenosis diagnosed during an abdominal exam?
What steps should be taken following an abdominal exam?
What is the role of an abdominal exam following surgery?
What is included in follow-up care after an abdominal exam?
What is included in patient education about abdominal exam?
Which tests and medications are indicated to confirm the physical findings of an abdominal exam?
-
Abdominal palpation of a boy.
-
Abdominal auscultation.
-
Abdominal auscultation.
-
Percussion over the liver.
-
Abdominal wall findings from a handlebar injury.
-
Abdominal wall findings in a passenger who was restrained with only a lap belt during a motor vehicle accident.
-
Location of McBurney point illustrated on the abdomen of a male subject.
-
Abdominal quadrants.
-
Grey Turner sign. This 40-year-old woman complained of worsening epigastric pain of five days' duration. On examination, she had hypotension, a board-like abdomen, and extensive ecchymoses over her right loin.
-
Acute pancreatitis with Cullen sign.
-
A person with jaundice due to hepatic failure.